August 11th, 2014 · Comments Off on Why Comprehensive Pain Treatment is Best
This article is part of our series How You Can Benefit from Psychiatric Pain Management.
Comprehensive pain treatment – seeing several different types of health care providers – works best. Why should you work with a health care team?
1. Pain is complicated and takes a team of experts to help get you better
Pain is complicated and is caused by many different factors. Unfortunately, there’s usually not 1 simple treatment that will cure you. However, on the positive side, that means there are multiple ways to improve things. Seeking different types of treatment – doctor, pain psychiatrist/psychologist, physical therapist, massage therapist, acupuncturist, etc. – lets each person add something to your treatment. Hopefully, all the treatments together get you to a better place. Many times treatments work in concert with each other. For example, anesthetic injections work better is you’re not overly anxious or depressed. So treating anxiety can help medication be more effective.
2. Working with a team lets each provider focus on what (s)he does best
In a sense, this is the flip-side of #1. It means that you utilize each person on your health care team to your best advantage. Your appointment times are not unlimited, so focusing in on what each person does best means you’re taking advantage of the expertise of each person. As a psychiatrist, I notice this issue most often related to anxiety or depression. If you’re seeing a psychiatrist or psychologist, you can work on these issues in therapy. This lets you spend your time with your medical pain management doctor (neurologist, anesthesiologist, rheumatologist, etc) talking about medications, injections and other procedures, instead of unloading your stress with them. Often they don’t have time to do both. So you get appropriate treatment, and they don’t get overwhelmed trying to treat problems they’re not equipped for.
2 studies that look at comprehensive treatment are:
- Rational integration of pharmacologic, behavioral and rehabilitation strategies in the treatment of chronic pain, Am J Phys Med Rehabil 2005, 84: S64-76
- Efficacy of multidisciplinary pain centers in the treatment of chronic pain, Prog Pain Res Manage 1996, 7:257-74
***To get every new article delivered to you for free the instant they're published, sign up for How to Cope with Pain by email or RSS feed.
Tags: 1
August 4th, 2014 · Comments Off on What is Psychiatric Pain Management?
This is a series about psychiatric pain management.
We’ll learn what it is and figure out if you might benefit from this treatment. If your doctor has recommended that you considering seeing a pain management psychiatrist or psychologist, it might not be clear exactly why this might be helpful. You might think, Does my doctor think my pain is all in my head? or, Will I have to lie on a couch and talk about my dreams?
The answer is no. No, it’s not all in your head. And, no, you’ll do other things instead of talking about your childhood.
There are many ways some visits to a pain management psychiatrist might be helpful. This is a psychiatrist who understands chronic pain, and who can teach you many ways to decrease and cope with pain. You want to look for someone who specifically has expertise in treating pain. This series will look at the benefits of this type of treatment.
***To get every new article delivered to you for free the instant they're published, sign up for How to Cope with Pain by email or RSS feed.
Tags: 1
June 30th, 2014 · Comments Off on Medications for Pain Series: Research Advances
This article is one in a series on Medications for Pain. What are your choices? How do various medications work? What are the pros and cons? How about side effects?
Here are 2 promising advances in research for pain.
1. The first advance is studying multiple medications together. As you might know all too well, it’s usually not a single medication alone which helps in chronic pain. Patients often use 2, 3, or even more medications together. However, most research looks at only 1 medication at a time. While this practice is simpler, it doesn’t help us know how to best combine medications for pain management.
Studies looking at more than 1 medication at a time are beginning to be published. Yay!! Here’s an example:
Lamotrigine in Combination with Other Medications for Neuropathic Pain. This study looked at adding lamotrigine (an anti-seizure medication) to either neurontin, a tricycle antidepressant, or another non-narcotic medication, in patients whose pain wasn’t well controlled with only 1 medication. The results showed that the addition of Lamotrigine didn’t help with pain.
As more studies are done, we’ll know better:
- what drugs to use together
- in what order to prescribe them
- what dosages to use together
(Study is: Silver M, Blum D, Grainger J, Hammer A, Quessy S, Double-blind, placebo-controlled trial of lamotrigine in combination with other medications for neuropathic pain. Journal of Pain and Symptom Management, Vol 34, 2007, 446-454.)
2. The second advance is studying medications for pain specifically and for particular pain disorders. National research organizations (eg NIH) as well as pharmaceutical companies are directing more dollars towards the study of pain. This will create advances in pain medicine – more options and quicker development of medication options. As well, specific pain disorders are being researched. For example, fibromyalgia has gone from being a questionable diagnosis to having multiple medications being approved to treat it.
***To get every new article delivered to you for free the instant they're published, sign up for How to Cope with Pain by email or RSS feed.
Tags: 1
June 23rd, 2014 · Comments Off on Medications for Pain Series: Medication Advances
This article is in a series on Medications for Pain. What are your choices? How do various medications work? What are the pros and cons? How about side effects?
What are some medication advances coming soon?
1. Improvements to opiates (narcotics)
While opiates or narcotics are sometimes helpful, they have more than their share of negatives. Selective narcotics, which give pain control but have fewer side effects, are being developed. Instead of working everywhere in the body, they’re being designed to work at pain sites, but not at so many other sites (for example, in your digestive tract) where they cause the problematic side effects. Another improvement is medication that will decrease side effects from opioids.
2. Different delivery systems for narcotics
Narcotics are being developed to be given either by inhalation (in inhalers, like asthma medication) or through the skin inside your mouth or nose (by rubbing a little gel there). Why? Medications used in these ways work faster and can last for a shorter time. These delivery systems may be very helpful for people who have break-through pain, which are short-duration spikes of pain. These short flares of pain can be hard to treat because medication didn’t work fast enough, or lasted too long. And, because of other advantages of getting medication into your body in these ways, lower overall dosages can be used, which also mean fewer side effects.
3. Using medications more safely
Research is being done to see how to use the medications we have now more safely. For narcotics, how do we avoid tolerance (tolerance = your body gets used to a dosage, so to get the same benefit, the dosage must increase). We’re finding that another pain medication, Ketamine, may be helpful to prevent tolerance.
4. Using genetics to predict which medication is right for you
Depression research is studying how genetics can predict which antidepressant is right for you. No guessing, no waiting – just a simple blood test which can be used to say, This one should work the best. We’re not at this stage yet with pain medication, but my hope is that such tests will be available soon. We could tell, Lyrica versus Neurontin? Cymbalta or Effexor? This would save a lot of time – not using medications which won’t work – and prevent a lot of side effects.
***To get every new article delivered to you for free the instant they're published, sign up for How to Cope with Pain by email or RSS feed.
Tags: 1
June 16th, 2014 · Comments Off on Medication for Pain Series: Antipsychotics
This article is in a series on Medications for Pain. What are your choices? How do various medications work? What are the pros and cons? How about side effects?
Antipsychotics are medications originally used for psychiatric disorders like schizophrenia or bipolar disorder, where a person’s thinking becomes disorganized or delusional.

Like many medication classes, antipsychotics aren’t FDA-approved for any pain disorders. There are only a few case reports of a single patient’s experience. So antipsychotics are not primary medications for pain.
Effect of Antipsychotics:
The only antipsychotic for which I could find any report of its use in pain is Zyprexa. Antipsychotics such as Zyprexa effect many neurotransmitter systems, including dopamine and serotonin, so it’s not clear where its pain-relieving effect comes from. As well, antipsychotics typically cause sedation, so some wonder if they help mainly through improving a patient’s sleep.
Side Effects:
- sedation (which can be helpful at night)
- dry mouth
- dizziness
- weight gain
- metabolic syndrome in some patients, which includes weight gain, increased blood pressure, and elevated cholesterol and triglycerides
Specific Pain Disorders
In these case studies, Zyprexa had a positive effect when used for both neuropathic pain disorders and rheumatoid arthritis (RA), an inflammatory pain disorder. This is quite interesting, as these are 2 different types of pain disorders. A medication more commonly works in 1 type of pain only. For example, anti-inflammatory medication works in RA, but not neuropathic pain disorders, such as diabetic pain.
While these medications may be worthwhile to study for their effect on pain, currently they should only be used when other more traditional medication has not worked.
***To get every new article delivered to you for free the instant they're published, sign up for How to Cope with Pain by email or RSS feed.
Tags: 1
June 9th, 2014 · Comments Off on Medications for Pain: Opiates
This article is in our series on Medications for Pain. What are your choices? How do various medications work? What are the pros and cons? How about side effects?
Opiate medication, sometimes called narcotics are medications designed to treat both acute and chronic pain. Of all medications for pain, narcotics probably get the most press and cause the most controversy. If you judged how important or effective narcotics were based on how much is written about them, you’d assume they were the primary treatment for pain.
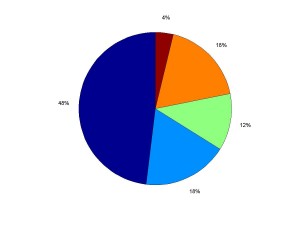
Instead, you’re probably better off if your medication regimen for chronic pain looks like this:
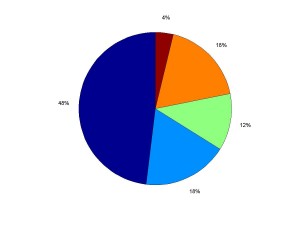
If used for chronic pain, narcotics should be 1 medication in an array of helpful treatments.
Narcotics:
Narcotics include opium derivatives (Morphine and Codeine) and synthetic opiates (Methadone, Demerol, Oxycodone).
Effect of Narcotics:
Narcotics work at opioid receptors, where they interfere and stop the transmission of pain messages to the brain. They also alter your psychological reaction to pain. Patients sometimes report still being aware of pain, but not having such an aversion to the feeling.
Side Effects:
- sedation
- nausea or vomiting
- constipation
- breathing difficulty at higher dosages
Issues with Narcotics
1. Effectiveness
While narcotics are great for acute pain, they often don’t work so well for chronic pain, especially nerve pain. The negative side effects can be greater than the good effects, making them not worth taking.
2. Tolerance
Over time, your body gets used to their effect. So to get the same benefit, a higher and higher dose is needed. Unfortunately, the side effects continue to increase too. However, don’t mistake tolerance, which is simply a physical process, with addiction.
3. Addiction
True addiction is a disease in which people continue to use a substance (alcohol, street drugs or prescription drugs), despite bad consequences such as physical illness, relationship problems or inability to function at work. Just because your body is tolerant to a medication, it doesn’t mean you’re addicted. Addiction is a behavior; tolerance is a physical process. However, a percentage of patients who use narcotics will develop true addiction, with symptoms such as lying about how much medication they’re using, doctor shopping to get more prescriptions, obtaining narcotics illegally, and using the medication to get high rather than to control pain. This may be a more likely possibility than previously thought, as seen in our current opiate epidemic. The risk is higher in people who’ve been addicted to drugs or alcohol in the past, and for those who have few other coping skills to deal with pain.
4. Side Effects
Side effects of narcotics can be significant. The most bothersome ones are usually sedation, slowed thinking, and constipation, which can be severe.
5. Do Narcotics Increase Pain?
An under-recognized problem is that for some people, narcotics can set up a process where pain will increase over time, even if the medication initially decreases pain. Narcotics can cause what’s call hyperalgesia, which is an increase in pain sensations. When this occurs, sometimes doctors think the medication isn’t working and increase the narcotic, when in fact the narcotic itself is increasing pain. A vicious cycle can develop. As with all drugs, for narcotics to continue to be prescribed, it should be clear that they’re decreasing pain.
Conclusion: Pain is bad, and sometimes narcotics are helpful and should be used. Doctors and patients need to be sure that the benefits are worth the risks or are greater than the side effects. When narcotics are used, it’s important to see if a person’s functioning is also improved, in addition to a decrease in pain.
***To get every new article delivered to you for free the instant they're published, sign up for How to Cope with Pain by email or RSS feed.
Tags: 1
June 2nd, 2014 · Comments Off on Medications for Pain Series: Blood Pressure Medication
This article is one in a series on Medications for Pain. What are your choices? How do various medications work? Pros and cons? How about side effects?
Anti-Hypertensive Medication are drugs originally used to control high blood pressure. A common medication from this class that’s used for pain is Clonidine.
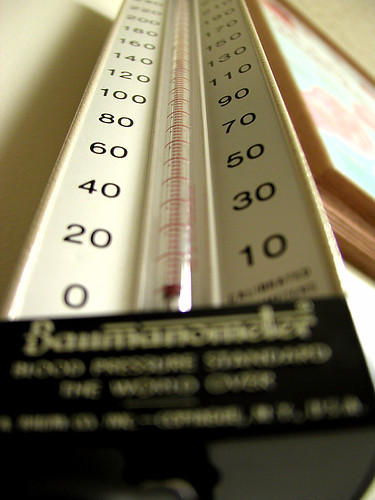
Like muscle relaxants, anti-hypertensives indirectly decrease pain. They would be considered supplemental medications for pain, rather than primary ones.
Effect of Anti-Hypertensives:
These medications work by decreasing the activity of your sympathetic nervous system. This is the fight or flight system in your body, the one that’s responsible for getting your body going – raising your blood pressure and getting your heart beating faster.
Uses of Anti-Hypertensives:
In some pain disorders, it’s thought that an overactive sympathetic system may be partly responsible for symptoms. CRPS (RSD) and other neuropathic pain disorders are some examples. Using anti-hypertensives in pain isn’t FDA-approved, but there are some studies supporting the use of these medications for pain.
Side Effects:
- a decrease in blood pressure (which is a direct effect of the medication, but is considered a side effect when the medication is used for pain control, as that’s not the effect that’s necessarily desired)
- sedation
- dizziness or lightheadedness
***To get every new article delivered to you for free the instant they're published, sign up for How to Cope with Pain by email or RSS feed.
Tags: 1
May 27th, 2014 · Comments Off on Medications for Pain Series: Muscle Relaxants
This article is one in a series on Medications for Pain. What are your choices? How do various medications work? Pros and cons? How about side effects?
Muscle Relaxants are drugs which help muscles relax and prevent muscle spasms. Common medications include Zanaflex and Baclofen.

Some medications such anticonvulsants and antidepressants can directly reduce pain. Most muscle relaxants work indirectly on pain, although Baclofen may also have direct pain-reducing effects. There are many categories of muscle relaxants, all working on different neurotransmitter systems in the body. We think of muscle relaxants as supplemental medications for pain, rather than primary ones.
Uses of Muscle Relaxants:
Muscle relaxants are used in conditions where these symptoms are a problem:
- muscle tension
- muscle spasm
- dystonia (severe, long-lasting spasm)
These symptoms can occur in pain disorders such as chronic back pain and CRPS.
Side Effects:
Side effects include sedation and weakness.
***To get every new article delivered to you for free the instant they're published, sign up for How to Cope with Pain by email or RSS feed.
Tags: 1
May 19th, 2014 · Comments Off on Medication for Pain Series: Ketamine
This article is in our series on Medications for Pain. What are your choices? How do various medications work? What are the pros and cons? Side effects?
The medication Ketamine is an anesthetic. Anesthetics are drugs which prevent sensations, particularly pain. Ketamine is an NMDA-receptor antagonist. Also in this class is Dextromethorophan (which is an active ingredient in cough syrup). These medications can be used:
- Topically (through the skin)
- By mouth in pill form
- Intravenous (IV) low-dose or moderate-dose infusion
- Intravenous (IV) at high doses (“ketamine coma”)
One study showed that moderate-dose infusions give much better pain relief than low-dose infusions do, without additional side effects, and so moderate-dosages are now recommended.
Effect of Ketamine:
Ketamine and others in this class are called NMDA-receptor antagonists. This means they block nerve conduction at a specific (NMDA) neurotransmitter site.
Uses of Ketamine:
Ketamine is only approved as an anesthetic for surgical procedures, not for chronic pain. In chronic pain treatment, it’s used on the skin for nerve pain, and by IV for CRPS (Complex Regional Pain Syndrome or RSD). Dextromethorophan, when used for chronic pain, is given in concentrated pill form, as the amount in cough syrup is very low.
Side Effects:
Ketamine’s short term side-effects include anxiety and hallucinations. There’s been concern over unknown longer-term consequences, including cognitive (memory) problems. However, one study showed no decrease in attention, learning, and memory in 9 patients with CRPS who underwent a Ketamine coma. Although we’re still at an early stage in learning how to use Ketamine more safely for chronic pain, I’m becoming a bigger fan of this treatment for use after other treatments have not been effective.
Also Interesting:
Ketamine’s other uses include in veterinary medicine, battlefield medicine, and as a recreational drug.
***To get every new article delivered to you for free the instant they're published, sign up for How to Cope with Pain by email or RSS feed.
Tags: 1
May 12th, 2014 · Comments Off on Medication for Pain Series: Anesthestics
This article is in our series on Medications for Pain. What are your choices? How do various medications work? Pros and cons? How about side effects?
Anesthetics are medications used to prevent sensations, particularly pain. Within this class, there are many different medications, and many ways to use these medications, including:
- Topical (through the skin), for example, a lidocaine patch. This delivers the anesthetic to nerves near the skin which are irritated. It can stay on for 12 hours or more, so you get a much longer effect than a cream.
- By mouth in pill form.
- Injection, either at a local site (local anesthesia) or covering a broader area (regional anesthesia). For injections, the anesthetic is often combined with a steroid medication.
- Intravenous (IV), for which an inpatient or outpatient hospital stay is needed.
Effect of Anesthetics: Anesthetics work by stabilizing nerve membranes, so it’s more difficult to transmit nerve signals, including pain signals.
Uses of Anesthetics: Although anesthetics are commonly used, there are few FDA-approved indications for anesthetics in specific pain disorders. The Lidoderm patch is FDA-approved for the pain of shingles (Post Herpetic Neuralgia). It’s also used for many other conditions, e.g. CRPS (Complex Regional Pain Disorder or RSD), diabetic nerve pain (Diabetic Peripheral Neuropathy), low back pain, etc. Local or regional injections are used for low back pain, other spinal pain, CRPS, etc.
Side Effects: Anesthetics used on the skin can cause skin irritation, either because of the anesthetic itself or the adhesive in the patch. Injections often cause temporary site irritation, either from the medication which is injected, or simply from injecting liquid inside your body. By their very nature, injections are also imprecise, even when your doctor uses fluoroscopy to guide the needle. Too far away from the right spot and the injection may not be effective. Too close, especially to a major nerve, and more significant nerve irritation and pain can result.
IV anesthetics can cause a drop in blood pressure or heart beat irregularities, so these must be monitored during the infusion.
Cost and Insurance Coverage
Insurance coverage for IV anesthetic treatment, for example, a lidocaine or ketamine infusion, can be very expensive. The cost is primarily for the hospital charges rather than the medication itself. However, as these treatments are in some cases very helpful, having your doctor go to bat for you with your insurance company to get them to pay for it is crucial for most patients.
***To get every new article delivered to you for free the instant they're published, sign up for How to Cope with Pain by email or RSS feed.
Tags: 1